ERCP fasaha ce mai mahimmanci don ganowa da magance cututtukan biliary da pancreas. Da zarar ta fito, ta samar da sabbin dabaru da yawa don magance cututtukan biliary da pancreas. Ba wai kawai ta "radiyo" ba ce. Ta canza daga fasahar ganewar asali zuwa sabuwar nau'in. Dabaru na magani sun haɗa da sphincterotomy, cire duwatsun bututun bile, magudanar ruwa da sauran hanyoyin magance cututtukan bile da pancreas.
Nasarar shigar bututun bile na zaɓi don ERCP na iya kaiwa sama da kashi 90%, amma har yanzu akwai wasu lokuta inda wahalar shiga bututun bile ke haifar da gazawar shigar bututun bile na zaɓi. Dangane da sabuwar yarjejeniya kan ganewar asali da magani na ERCP, ana iya bayyana shigar bututun bile mai wahala kamar haka: lokacin shigar bututun bile na zaɓi na babban kan nono na ERCP na yau da kullun ya fi mintuna 10 ko adadin ƙoƙarin shigar bututun bile ya fi sau 5. Lokacin yin ERCP, idan shigar bututun bile yana da wahala a wasu lokuta, ya kamata a zaɓi dabarun da suka dace akan lokaci don inganta ƙimar nasarar shigar bututun bile. Wannan labarin yana gudanar da bita mai tsari na dabarun shigar bututun bile da yawa da ake amfani da su don magance matsalar shigar bututun bile, da nufin samar da tushen ka'ida ga masu binciken endoscopists na asibiti don zaɓar dabarun amsawa lokacin da ake fuskantar wahalar shigar bututun bile don ERCP.
I. Fasahar Wayar Jagora Guda ɗaya, SGT
Dabarar SGT ita ce amfani da na'urar auna zafin jiki don ci gaba da ƙoƙarin shigar da bututun bile bayan wayar jagora ta shiga bututun pancreas. A farkon zamanin haɓaka fasahar ERCP, SGT hanya ce da aka saba amfani da ita don magance matsalar shigar da bututun bile. Amfaninta shine cewa yana da sauƙin aiki, yana gyara kan nono, kuma yana iya mamaye buɗe bututun pancreas, wanda hakan ke sauƙaƙa samun buɗe bututun bile.
Akwai rahotanni a cikin adabi cewa bayan rashin nasarar shigar da allurar rigakafi ta al'ada, zaɓar shigar da allurar rigakafi ta SGT-assisted na iya kammala shigar da allurar rigakafi ta hanyar bile duct a cikin kusan kashi 70%-80% na lokuta. Rahoton ya kuma nuna cewa a cikin yanayin rashin nasarar SGT, har ma da daidaitawa da amfani da allurar rigakafi sau biyu.waya mai jagorafasahar ba ta inganta nasarar shigar da bututun bile ba kuma ba ta rage yawan kamuwa da cutar pancreatitis bayan ERCP (PEP) ba.
Wasu bincike sun kuma nuna cewa nasarar da aka samu wajen shigar da SGT ta hanyar intubation ya yi ƙasa da na sau biyu.waya mai jagorafasaha da fasahar transpancreatic papillary sphincterotomy. Idan aka kwatanta da yunƙurin SGT da aka maimaita, aiwatar da farko na biyuwaya mai jagorafasahar fasaha ko fasahar kafin yankewa na iya samun sakamako mafi kyau.
Tun bayan haɓaka ERCP, an ƙirƙiri sabbin fasahohi iri-iri don wahalar shigar da bututun ciki. Idan aka kwatanta da injin guda ɗaya.waya mai jagorafasaha, fa'idodin sun fi bayyana kuma ƙimar nasara ta fi girma. Saboda haka, guda ɗayawaya mai jagoraA halin yanzu ba kasafai ake amfani da fasahar a asibiti ba.
II.Tsarin waya mai jagora biyu,DGT
Ana iya kiran DGT hanyar amfani da wayar da aka yi amfani da ita wajen shigar da bututun pancreas, wato barin wayar jagora ta shiga bututun pancreas don bibiya da mamaye shi, sannan a sake amfani da wayar jagora ta biyu a saman wayar jagorar bututun pancreas. Shigar da bututun bile na zaɓi.
Amfanin wannan hanyar sune:
(1) Tare da taimakon waniwaya mai jagoraBuɗewar bututun bile ya fi sauƙi a samu, yana sa bututun bile ya yi laushi;
(2) Wayar jagora za ta iya gyara nonon;
(3) Karkashin jagorancin bututun pancreaswaya mai jagora, ana iya guje wa sake ganin bututun pancreas, ta haka ne za a rage motsin bututun pancreas wanda ke faruwa sakamakon yawan shigar ciki.
Dumonceau da abokan aikinsa sun lura cewa ana iya saka wayar jagora da kuma catheter mai kama da juna a cikin ramin biopsy a lokaci guda, sannan suka bayar da rahoton nasarar da aka samu a hanyar da aka bi wajen shigar da wayar jagora a cikin bututun pancreas, kuma suka kammala da cewawaya mai jagorashan hanyar bututun pancreas ya yi nasara wajen shigar da bututun bile. rate yana da tasiri mai kyau.
Wani bincike da Liu Deren da abokan aikinsa suka gudanar kan DGT ya gano cewa bayan an yi wa marasa lafiya da ke fama da matsalar toshewar bututun bile na ERCP, nasarar shigar da DGT ta kai kashi 95.65%, wanda ya fi yawa fiye da kashi 59.09% na nasarar shigar da DGT ta al'ada.
Wani bincike da Wang Fuquan da abokan aikinsa suka gudanar ya nuna cewa lokacin da aka yi amfani da DGT ga marasa lafiya da ke fama da matsalar shigar da bututun bile na ERCP a cikin rukunin gwaji, nasarar shigar da allurar ta kai kashi 96.0%.
Nazarin da ke sama ya nuna cewa amfani da DGT ga marasa lafiya da ke da wahalar shigar da bututun bile don ERCP na iya inganta nasarar shigar da bututun bile yadda ya kamata.
Rashin kyawun DGT ya haɗa da waɗannan abubuwa guda biyu:
(1) Ciwon pancreaswaya mai jagorawatakila ya ɓace yayin shigar da bututun bile, ko kuma na biyuwaya mai jagorazai iya sake shiga cikin bututun pancreas;
(2) Wannan hanyar ba ta dace da shari'o'i kamar ciwon daji na kan pancreas, tortuosity na bututun pancreas, da kuma fission na pancreas ba.
Daga mahangar kamuwa da cutar PEP, yawan kamuwa da cutar PEP na DGT ya yi ƙasa da na kamuwa da cutar ta hanyar bututun bile na al'ada. Wani bincike da aka yi kwanan nan ya nuna cewa yawan kamuwa da cutar PEP bayan DGT ya kai kashi 2.38% kacal a cikin marasa lafiya na ERCP da ke fama da matsalar toshewar bututun bile. Wasu wallafe-wallafe sun nuna cewa duk da cewa DGT tana da mafi girman nasarar toshewar bututun bile, yawan kamuwa da cutar pancreatitis bayan DGT har yanzu ya fi yawa idan aka kwatanta da sauran matakan gyara, saboda aikin DGT na iya haifar da lalacewa ga bututun pancreas da buɗewar sa. Duk da haka, yarjejeniya a cikin gida da ƙasashen waje har yanzu tana nuna cewa a cikin yanayin toshewar bututun bile mai wahala, lokacin da toshewar bututun ke da wahala kuma bututun pancreas akai-akai ana kuskuren shigar da shi, DGT shine zaɓi na farko saboda fasahar DGT ba ta da wahalar aiki, kuma tana da sauƙin sarrafawa. Ana amfani da ita sosai a cikin toshewar bututu mai wahala.
III. Jagorar waya ta cannulation-pan-creatic stent, WGC-P5
Ana iya kiran WGC-PS da hanyar occupation stent duct duct. Wannan hanyar ita ce a sanya stent duct duct tare dawaya mai jagorawanda ke shiga cikin bututun pancreas ba bisa kuskure ba, sannan ya cirewaya mai jagorakuma a yi aikin toshe bututun bile a saman stent.
Wani bincike da Hakuta da abokan aikinsa suka gudanar ya nuna cewa baya ga inganta nasarar shigar da bututun ta hanyar jagorantar shigar da bututun ta hanyar amfani ...
Wani bincike kan WGC-PS da Zou Chuanxin da abokan aikinsa suka yi ya nuna cewa nasarar da aka samu wajen shigar da bututun ciki ta hanyar amfani da hanyar wucin gadi ta hanyar amfani da bututun pancreas ya kai kashi 97.67%, kuma yawan PEP ya ragu sosai.
Wani bincike ya gano cewa idan aka sanya stent na bututun pancreas daidai, yuwuwar kamuwa da cutar pancreatitis mai tsanani bayan tiyata a cikin mawuyacin hali na intubation yana raguwa sosai.
Wannan hanyar har yanzu tana da wasu kurakurai. Misali, bututun pancreas da aka saka a lokacin aikin ERCP na iya zama naƙasa; idan ana buƙatar sanya stent na dogon lokaci bayan ERCP, za a sami babban yuwuwar toshewar stent da toshewar bututu. Rauni da sauran matsaloli suna haifar da ƙaruwar yawan PEP. Tuni, cibiyoyi sun fara nazarin bututun pancreas na ɗan lokaci waɗanda za su iya fita daga bututun pancreas kai tsaye. Manufar ita ce amfani da bututun pancreas don hana PEP. Baya ga rage yawan haɗarin PEP sosai, irin waɗannan stents kuma za su iya guje wa wasu ayyuka don cire stent da rage nauyin da ke kan marasa lafiya. Duk da cewa bincike ya nuna cewa bututun pancreas na ɗan lokaci yana da tasiri mai kyau wajen rage PEP, aikace-aikacen su na asibiti har yanzu yana da manyan ƙuntatawa. Misali, a cikin marasa lafiya da siraran bututun pancreas da rassan da yawa, yana da wuya a saka stent bututun pancreas. Matsalar za ta ƙaru sosai, kuma wannan aikin yana buƙatar ƙwararren masanin endoscope. Ya kamata a lura cewa stent ɗin bututun pancreas da aka sanya bai kamata ya yi tsayi sosai a cikin duodenal lumen ba. Stent mai tsayi da yawa na iya haifar da huda duodenal. Saboda haka, zaɓin hanyar mamaye bututun pancreas har yanzu yana buƙatar kulawa da hankali.
IV. Trans-pancreatocsphincterotomy,TPS
Ana amfani da fasahar TPS gabaɗaya bayan wayar jagora ta shiga bututun pancreas bisa kuskure. Ana yanke septum ɗin da ke tsakiyar bututun pancreas tare da alkiblar wayar jagora ta bututun pancreas daga ƙarfe 11 zuwa 12, sannan a saka bututun a alkiblar bututun bile har sai wayar jagora ta shiga bututun bile.
Wani bincike da Dai Xin da abokan aikinsa suka gudanar ya kwatanta TPS da wasu fasahohin intubation guda biyu. Ana iya ganin cewa nasarar fasahar TPS tana da girma sosai, inda ta kai kashi 96.74%, amma ba ta nuna sakamako mai kyau ba idan aka kwatanta da sauran fasahohin intubation guda biyu. Fa'idodin.
An ruwaito cewa halayen fasahar TPS sun haɗa da waɗannan abubuwan:
(1) Yankewar ƙanƙanta ce ga septum na pancreasobiliary;
(2) Yawan matsalolin bayan tiyata ba shi da yawa;
(3) Zaɓin hanyar yankewa abu ne mai sauƙin sarrafawa;
(4) Ana iya amfani da wannan hanyar ga marasa lafiya da ke fama da maimaita shigar bututun pancreas ko kuma kan nono a cikin diverticulum.
Nazarce-nazarce da yawa sun nuna cewa TPS ba wai kawai zai iya inganta nasarar shigar bututun bile cikin sauƙi ba, har ma ba ya ƙara yawan rikice-rikice bayan ERCP. Wasu masana sun ba da shawarar cewa idan shigar bututun pancreas ko ƙaramin papilla na duodenal ya faru akai-akai, ya kamata a fara la'akari da TPS. Duk da haka, lokacin amfani da TPS, ya kamata a mai da hankali kan yiwuwar toshe bututun pancreas da sake dawowar pancreatitis, waɗanda ke iya zama haɗarin dogon lokaci na TPS.
V. Precut Sphincterotomy, PST
Dabarar PST tana amfani da madaurin papillary arcuate a matsayin iyakar sama ta kafin yankewa da kuma alkiblar ƙarfe 1-2 a matsayin iyaka don buɗe duodenal papilla sphincter don nemo buɗewar bile da pancreas duct. A nan PST musamman yana nufin dabarar pre-incision sphincter na nono ta amfani da wuka mai arcuate. A matsayin dabarar magance matsalar intubation na bile duct don ERCP, an yi la'akari da fasahar PST a matsayin zaɓi na farko don wahalar intubation. Pre-incision na nono na endoscopic yana nufin yanke endoscopic na mucosa na saman papilla da ƙaramin adadin tsokar sphincter ta hanyar wukar yankewa don nemo buɗewar bile duct, sannan amfani dawaya mai jagorako kuma catheter don shigar da bututun bile.
Wani bincike na cikin gida ya nuna cewa nasarar PST ta kai kashi 89.66%, wanda ba shi da bambanci sosai da DGT da TPS. Duk da haka, yawan PEP a cikin PST ya fi na DGT da TPS girma sosai.
A halin yanzu, shawarar amfani da wannan fasahar ta dogara ne akan dalilai daban-daban. Misali, wani rahoto ya bayyana cewa PST ya fi dacewa a yi amfani da shi a lokuta inda papilla na duodenal ya kasance ba daidai ba ko kuma ya karkace, kamar stenosis na duodenal ko malignancy.
Bugu da ƙari, idan aka kwatanta da sauran dabarun magance matsalar, PST tana da yawan aukuwar matsaloli kamar PEP, kuma buƙatun tiyata suna da yawa, don haka wannan tiyatar ta fi dacewa ta hanyar ƙwararrun masu duba lafiyar kwakwalwa.
VI. Wukar allura Papillotomy,NKP
NKP wata dabara ce ta shigar da allura da wuka. Idan shigar da allurar ta yi wahala, ana iya amfani da wuka mai allura don yanke wani ɓangare na papilla ko sphincter daga buɗewar papilla ta duodenal a kusurwar ƙarfe 11-12, sannan a yi amfani dawaya mai jagorako kuma catheter zuwa Selective insertion a cikin hanyar bile duct na gama gari. A matsayin dabarun magance matsalar intubation na hanyar bile duct mai wahala, NKP na iya inganta nasarar intubation mai wahala na hanyar bile duct yadda ya kamata. A baya, an yi imanin cewa NKP zai ƙara yawan PEP a cikin 'yan shekarun nan. A cikin 'yan shekarun nan, rahotannin bincike da yawa da aka yi nazari a kansu sun nuna cewa NKP ba ya ƙara haɗarin rikitarwa bayan tiyata. Yana da kyau a lura cewa idan an yi NKP a farkon matakin intubation mai wahala, zai taimaka sosai wajen inganta nasarar intubation. Duk da haka, a halin yanzu babu wata yarjejeniya kan lokacin da za a yi amfani da NKP don cimma mafi kyawun sakamako. Wani bincike ya ruwaito cewa yawan intubation na NKP ya yi amfani da shi a lokacinERCPƙasa da minti 20 ya fi na NKP da aka yi amfani da shi bayan mintuna 20.
Marasa lafiya da ke fama da matsalar toshewar bututun bile za su fi amfana daga wannan dabarar idan suna da kumburin nono ko kuma faɗaɗa bututun bile sosai. Bugu da ƙari, akwai rahotannin cewa idan aka fuskanci matsalolin toshewar hanji, haɗakar amfani da TPS da NKP yana da mafi girman nasarar fiye da shafa shi kaɗai. Rashin kyawunsa shine cewa dabarun yankewa da yawa da aka yi amfani da su a kan nono zai ƙara yawan faruwar matsaloli. Saboda haka, ana buƙatar ƙarin bincike don tabbatar da ko za a zaɓi yankewa da wuri don rage faruwar rikitarwa ko kuma a haɗa matakan gyara da yawa don inganta ƙimar nasarar toshewar hanji mai wahala.
VII.Needle-wuka Fistulotomy,NKE
Dabarar NKF tana nufin amfani da wukar allura don huda mucosa kimanin 5mm sama da kan nono, ta amfani da gaurayen wutar lantarki don huda layi-layi a alkiblar ƙarfe 11 har sai an sami tsarin da ke kama da saman ko kuma kwararar bile, sannan a yi amfani da wayar jagora don gano fitar bile da yanke nama. An yi amfani da hanyar shigar da bututun bile a wurin jaundice. An yi tiyatar NKF a saman buɗewar kan nono. Saboda kasancewar sinus na bututun bile, yana rage lalacewar zafi da lalacewar injiniya ga buɗe bututun pancreas sosai, wanda zai iya rage yawan faruwar PEP.
Wani bincike da Jin da abokan aikinsa suka gudanar ya nuna cewa nasarar shigar bututun NK zai iya kaiwa kashi 96.3%, kuma babu PEP bayan tiyata. Bugu da ƙari, nasarar NKF a cire dutse ya kai kashi 92.7%. Saboda haka, wannan binciken ya ba da shawarar NKF a matsayin zaɓi na farko don cire dutse na bututun bile. Idan aka kwatanta da papillomyotomy na gargajiya, haɗarin aikin NKF har yanzu yana da yawa, kuma yana iya fuskantar matsaloli kamar hudawa da zubar jini, kuma yana buƙatar babban matakin aiki na endoscopy. Wurin buɗe taga daidai, zurfin da ya dace, da kuma dabarar da ta dace duk suna buƙatar a koya a hankali. Kwarewa.
Idan aka kwatanta da sauran hanyoyin kafin yankewa, NKF hanya ce mafi dacewa tare da ƙimar nasara mafi girma. Duk da haka, wannan hanyar tana buƙatar yin aiki na dogon lokaci da kuma ci gaba da tattarawa daga mai aiki don ya zama mai ƙwarewa, don haka wannan hanyar ba ta dace da masu farawa ba.
VIII. Maimaita-ERCP
Kamar yadda aka ambata a sama, akwai hanyoyi da yawa don magance matsalar shigar ciki. Duk da haka, babu tabbacin nasara 100%. Littattafan da suka dace sun nuna cewa lokacin da shigar ciki ta hanyar bututun bile ke da wahala a wasu lokuta, shigar ciki ta dogon lokaci ko kuma tasirin shigar zafi na pre-cut na iya haifar da kumburin papilla na duodenal. Idan tiyatar ta ci gaba, shigar ciki ta hanyar bututun bile ba zai yi nasara ba, har ma da yuwuwar rikitarwa ma zai ƙaru. Idan yanayin da ke sama ya faru, za ku iya la'akari da dakatar da shigar ciki ta hanyarERCPA fara yin tiyata sannan a yi ERCP na biyu a lokaci na zaɓi. Bayan papilloedema ta ɓace, aikin ERCP zai fi sauƙi a cimma nasarar shigar da ciki.
Donnellan da sauransu sun yi na biyuERCPAn yi wa marasa lafiya 51 tiyatar da ERCP ta gaza bayan an yanke musu allurar riga-kafi, kuma an yi nasarar samun mutane 35 da suka kamu da cutar, kuma yawan matsalolin bai ƙaru ba.
Kim da abokan aikinsa sun yi tiyatar ERCP ta biyu a kan marasa lafiya 69 da suka gazaERCPBayan an yanke allura kafin a yi wa mutum tiyata, kuma an samu nasara a shari'o'i 53, inda aka samu nasara a shari'o'in da suka kai kashi 76.8%. Sauran shari'o'in da ba su yi nasara ba sun kuma yi tiyatar ERCP ta uku, inda aka samu nasara a shari'o'in da suka kai kashi 79.7%, kuma tiyata da yawa ba ta ƙara yawan faruwar matsaloli ba.
Yu Li da abokan aikinsa sun yi karatun sakandare na zaɓeERCPakan marasa lafiya 70 da suka kasa yin ERCP bayan an yanke musu allura kafin a yanke musu allura, kuma an samu nasarar shari'o'i 50. Jimillar nasarar (ERCP na farko + ERCP na biyu) ta karu zuwa 90.6%, kuma yawan rikice-rikicen bai karu sosai ba. . Duk da cewa rahotanni sun tabbatar da ingancin ERCP na biyu, tazara tsakanin ayyukan ERCP guda biyu bai kamata ta yi tsayi sosai ba, kuma a wasu lokuta na musamman, jinkirin fitar da biliary na iya kara ta'azzara yanayin.
IX. Magudanar ruwa ta biliary mai jagora ta hanyar amfani da na'urar duban dan tayi ta EUS-BD
EUS-BD wata hanya ce ta shiga tsakani wadda ke amfani da allurar hudawa don huda gallbladder daga ciki ko duodenum lumen a ƙarƙashin jagorancin duban dan tayi, sannan ta shiga duodenum ta cikin duodenal papilla, sannan ta yi aikin intubation na biliary. Wannan dabarar ta haɗa da hanyoyin intrahepatic da extrahepatic.
Wani bincike da aka yi a baya ya nuna cewa nasarar EUS-BD ta kai kashi 82%, kuma yawan matsalolin da suka faru bayan tiyata ya kai kashi 13% kacal. A wani bincike da aka yi, EUS-BD idan aka kwatanta da fasahar kafin yankewa, nasarar shigarta ta fi girma, inda ta kai kashi 98.3%, wanda ya fi kashi 90.3% na yankewa kafin yankewa. Duk da haka, zuwa yanzu, idan aka kwatanta da sauran fasahohi, har yanzu akwai karancin bincike kan amfani da EUS don matsaloli masu wahala.ERCPIntubation. Babu isassun bayanai da za su tabbatar da ingancin fasahar huda bututun bile da EUS ke jagoranta don magance matsalolin da ke tattare da amfani da shi.ERCPIntubation. Wasu bincike sun nuna cewa ya ragu. Matsayin PEP bayan tiyata ba shi da gamsarwa.
X. Magudanar ruwan hanji ta hanyar hanta, PTCD
PTCD wata hanya ce ta gwaji mai cin zarafi wadda za a iya amfani da ita tare daERCPdon wahalar shigar bututun bile, musamman a lokutan toshewar biliary mai tsanani. Wannan dabarar tana amfani da allurar huda don shiga bututun bile a hankali, huda bututun bile ta cikin papilla, sannan ta sake shigar da bututun bile ta hanyar da aka keɓe.waya mai jagoraWani bincike ya yi nazari kan marasa lafiya 47 da ke fama da matsalar toshewar bututun bile waɗanda aka yi musu dabarar PTCD, kuma nasarar ta kai kashi 94%.
Wani bincike da Yang da abokan aikinsa suka gudanar ya nuna cewa amfani da EUS-BD a bayyane yake yana da iyaka idan ana maganar stenosis na hilar da kuma buƙatar huda bututun bile na dama a cikin hanta, yayin da PTCD ke da fa'idodin daidaita tsarin bututun bile da kuma kasancewa mai sassauƙa a cikin na'urorin jagora. Ya kamata a yi amfani da bututun bile a cikin irin waɗannan marasa lafiya.
PTCD aiki ne mai wahala wanda ke buƙatar horo na dogon lokaci da kuma kammala isassun adadin shari'o'in da aka samu. Yana da wuya ga waɗanda ba su fara aiki su kammala wannan aikin ba. PTCD ba wai kawai yana da wahalar aiki ba ne, har ma yana da wahalar aiki.waya mai jagoraHakanan zai iya lalata bututun bile a lokacin ci gaba.
Duk da cewa hanyoyin da ke sama na iya inganta nasarar shigar da bututun bile cikin matsala, zaɓin yana buƙatar a yi la'akari da shi sosai.ERCP, SGT, DGT, WGC-PS da sauran dabarun za a iya la'akari da su; idan dabarun da ke sama suka gaza, ƙwararrun likitocin endoscopists na ƙwararru za su iya yin dabarun kafin yankewa, kamar TPS, NKP, NKF, da sauransu; idan har yanzu Idan ba za a iya kammala shigar da bututun bile na zaɓi ba, na biyu na zaɓiERCPza a iya zaɓarsa; idan babu ɗayan dabarun da ke sama da za su iya magance matsalar wahalar shigar da ciki, ana iya gwada ayyukan shiga kamar EUS-BD da PTCD don magance matsalar, kuma ana iya zaɓar maganin tiyata idan ya cancanta.
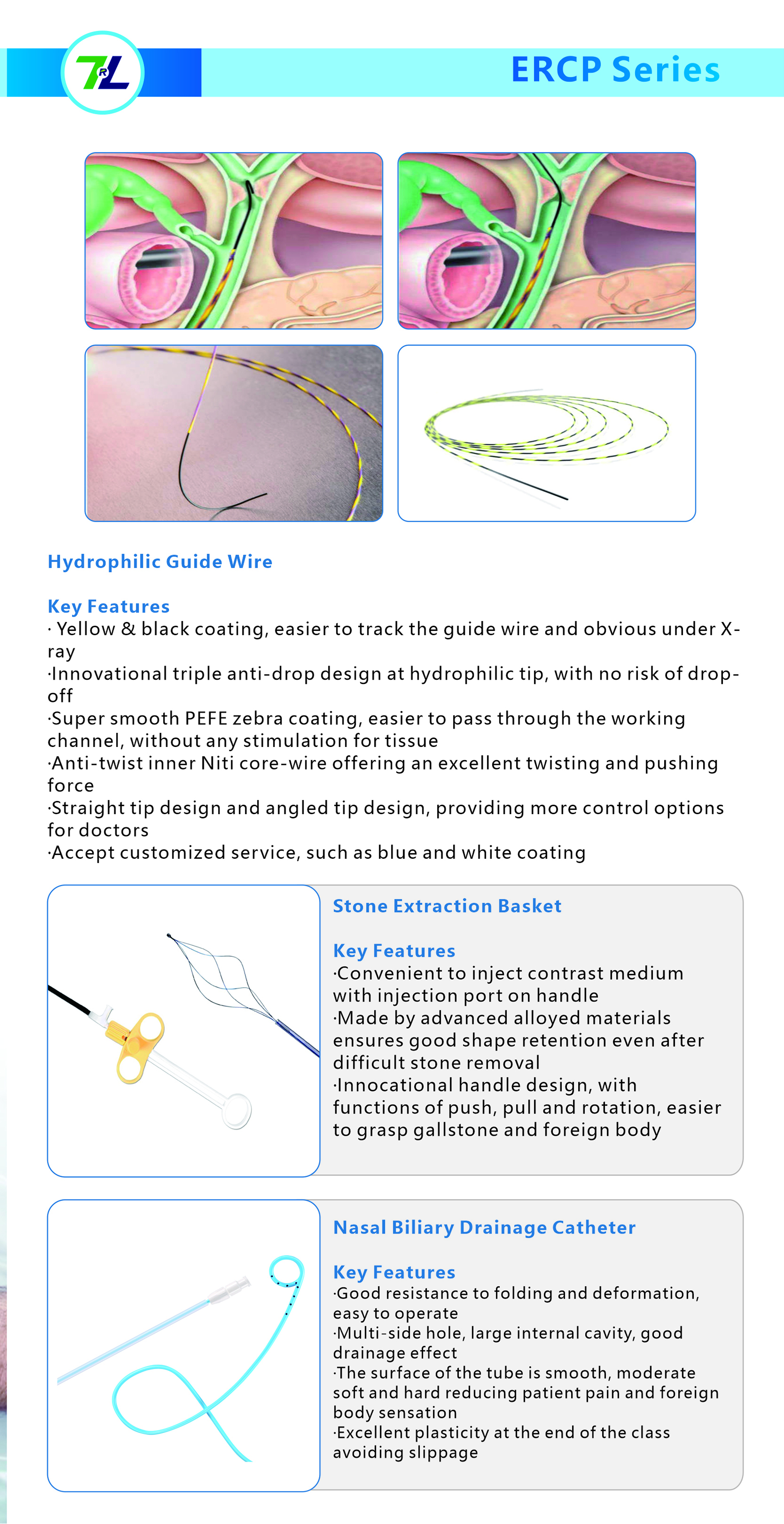
Mu, Jiangxi Zhuoruihua Medical Instrument Co., Ltd., kamfani ne da ke kera kayayyaki a China, wanda ya ƙware a fannin amfani da endoscopic, kamar su biopsy forceps, hemoclip, polyp snare, sclerotherapy allura, feshi catheter, gogaggun cytology,waya mai jagora, Kwandon ɗaukar dutse, catheter na magudanar ruwa ta hancida sauransu waɗanda ake amfani da su sosai a cikin EMR, ESD,ERCPKayayyakinmu an ba su takardar shaidar CE, kuma masana'antunmu an ba su takardar shaidar ISO. An fitar da kayayyakinmu zuwa Turai, Arewacin Amurka, Gabas ta Tsakiya da wani ɓangare na Asiya, kuma yana sa abokin ciniki ya yaba da kuma yaba masa sosai!
Lokacin Saƙo: Janairu-31-2024