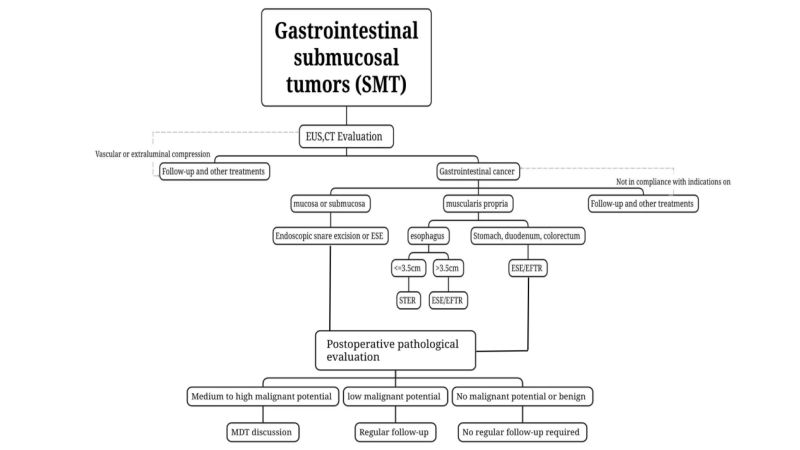
Ciwon daji na submucosal (SMT) na tsarin narkewar abinci raunuka ne masu tasowa waɗanda suka samo asali daga mucosa muscularis, submucosa, ko muscularis propria, kuma suna iya zama raunuka na waje. Tare da haɓaka fasahar likitanci, zaɓuɓɓukan maganin gargajiya sun shiga zamanin maganin da ba shi da tasiri sosai, kamar lTiyatar aparascopic da tiyatar robot. Duk da haka, a aikin asibiti, ana iya gano cewa "tiyata" ba ta dace da dukkan marasa lafiya ba. A cikin 'yan shekarun nan, ƙimar maganin endoscopic ta sami kulawa a hankali. An fitar da sabuwar sigar amincewa da ƙwararrun China kan ganewar endoscopic da maganin SMT. Wannan labarin zai ɗan ƙara koyo game da ilimin da ya dace.
1. Halin annobar SMTta'addanci
(1) Yawan kamuwa da cutar SMT ba shi da daidaito a sassa daban-daban na tsarin narkewar abinci, kuma ciki shine wurin da SMT ya fi yawa.
Yawan nau'ikan halittu daban-dabanSassan tsarin narkewar abinci ba su daidaita ba, inda tsarin narkewar abinci na sama ya fi yawa. Daga cikin waɗannan, kashi 2/3 na faruwa ne a cikin ciki, sai kuma esophagus, duodenum, da kuma hanji.
(2) Tarihin cutar kansaNau'ikan SMT l suna da rikitarwa, amma yawancin SMT raunuka ne marasa lahani, kuma kaɗan ne kawai ke da illa.
A.SMT ya haɗa da baburaunukan neoplastic kamar nama na pancreas da kuma raunukan neoplastic.
B. Daga cikin raunin neoplastics, leiomyomas na ciki, lipomas, Brucella adenomas, ciwace-ciwacen ƙwayoyin granulosa, schwannomas, da ciwace-ciwacen glomus galibi ba su da lahani, kuma ƙasa da kashi 15% na iya bayyana a matsayin kyallen takarda Koyi mugunta.
C. Ciwon ciki (stroma)ciwon daji (GIST) da ciwon daji na neuroendocrine (NET) a cikin SMT su ne ciwon daji masu wasu yiwuwar cutarwa, amma wannan ya dogara da girmansa, wurinsa da nau'insa.
D. Wurin da SMT yake yana da alaƙazuwa ga rarrabuwar cututtuka: a. Leiomyomas nau'in SMT ne da aka saba gani a cikin esophagus, wanda ya kai kashi 60% zuwa 80% na SMTs na esophagus, kuma yana iya faruwa a tsakiya da ƙananan sassan esophagus; b. Nau'ikan SMT na ciki suna da rikitarwa, tare da GIST, leiomyoMace da kuma ƙashin ƙugu su ne suka fi yawa. Daga cikin cututtukan ciki na SMT, GIST an fi samunsa a cikin fundus da jikin ciki, leiomyoma yawanci yana cikin zuciya da kuma sashin jiki na sama, kuma ƙashin ƙugu da ƙashin ƙugu sune suka fi yawa. Lipomas sun fi yawa a cikin antrum na ciki; c. Lipomas da cysts sun fi yawa a cikin sassan duodenum masu saukowa da bulbous; d. A cikin SMT na ƙananan hanyoyin ciki, lipomas sun fi yawa a cikin hanji, yayin da NETs suka fi yawa a cikin dubura.
(3) Yi amfani da CT da MRI don tantancewa, magancewa, da kuma tantance ciwace-ciwacen. Ga SMTs waɗanda ake zargin suna da yuwuwar zama masu illa ko kuma suna da manyan ciwace-ciwacen (dogon lokaci)diamita > 2 cm), CT da MRI ana ba da shawarar.
Sauran hanyoyin daukar hoto, gami da CT da MRI, suma suna da matukar muhimmanci wajen gano cutar SMT. Suna iya nuna kai tsaye wurin da ciwon ya faru, tsarin girma, girman rauni, siffa, kasancewar ko rashin lobulation, yawan abu, daidaito, matakin haɓakawa, da kuma yanayin iyaka, da sauransu, kuma suna iya gano ko da matakin kauri ne.Taɓarɓarewar bangon hanji. Mafi mahimmanci, waɗannan gwaje-gwajen hoto na iya gano ko akwai mamayewar tsarin raunin da ke maƙwabtaka da kuma ko akwai metastasis a cikin peritoneum, lymph nodes da sauran gabobin da ke kewaye. Su ne babbar hanyar tantancewa ta asibiti, magani da kuma tantance hasashen ciwace-ciwacen.
(4) Samfuran nama ba a sake shi baAna yin gwajin ne don gano cututtukan SMT marasa kyau waɗanda za a iya gano su ta hanyar amfani da endoscopy na gargajiya tare da EUS, kamar lipomas, cysts, da ectopic pancreas.
Ga raunukan da ake zargin suna da illa ko kuma lokacin da endoscopy na gargajiya tare da EUS ba za su iya tantance raunukan marasa lahani ko masu cutarwa ba, ana iya amfani da gwajin allura/biopsi na EUS wanda aka shirya (duba hoton duban dan tayi na endoscopic wanda aka shirya fine nAspiration/Biopsy na eedle, EUS-FNA/FNB), biopsy na yanke mucosal (biopsy mai taimako ga yanke mucosalinced, MIAB), da sauransu. yi samfurin biopsy don kimanta cututtukan da suka shafi aikin tiyata. Ganin iyakokin EUS-FNA da tasirin da ke biyo baya akan cire endoscopic, ga waɗanda suka cancanci yin tiyatar endoscopic, bisa ga tabbatar da cewa za a iya cire ƙari gaba ɗaya, ƙwararrun masu fasaha na maganin endoscopic za su iya magance na'urori masu fasahar maganin endoscopic masu girma. Likitan endoscopic yana yin tiyatar endoscopic kai tsaye ba tare da samun ganewar cutar kafin tiyata ba.
Duk wata hanyar samun samfuran cututtuka kafin tiyata tana da illa kuma za ta lalata mucosa ko kuma ta haifar da mannewa ga kyallen da ke ƙarƙashin mucosa, ta haka za ta ƙara wahalar tiyata da kuma yiwuwar ƙara haɗarin zubar jini.Rarraba ƙwayoyin cuta, da kuma yaɗuwar ƙari. Saboda haka, ba lallai ba ne a yi amfani da biopsy kafin tiyata. Dole ne, musamman ga SMTs waɗanda za a iya gano su ta hanyar amfani da endoscopy na gargajiya tare da EUS, kamar lipomas, cysts, da ectopic pancreas, ba a buƙatar ɗaukar samfurin nama.
2. Jiyya ta endoscopic ta SMTnt
(1) Ka'idojin magani
Raunukan da ba su da metastasis na ƙwayoyin lymph nodes ko kuma ƙarancin haɗarin metastasis na ƙwayoyin lymph nodes, ana iya cire su gaba ɗaya ta amfani da dabarun endoscopic, kuma suna da ƙarancin haɗarin sake dawowa sun dace da cirewar ƙwayoyin lymph idan magani ya zama dole. Cire ƙari gaba ɗaya yana rage sauran ciwon da kuma haɗarin sake dawowa.Ya kamata a bi ƙa'idar maganin da ba shi da ƙari yayin cirewar endoscopic, kuma ya kamata a tabbatar da ingancin ƙwayar ciwon yayin cirewar.
(2) Alamomi
i. Cututtuka masu yuwuwar cutarwa da ake zargi da su ta hanyar gwajin kafin tiyata ko kuma an tabbatar da su ta hanyar binciken biopsy, musamman waɗanda ake zargi da cutar GI.Ana iya cire ST ɗin kafin tiyatar tsawon ciwon da ya kai ≤2cm da ƙarancin haɗarin sake dawowa da kuma kamuwa da cutar, kuma tare da yuwuwar cire cikakken sashi, ta hanyar amfani da endoscopic; ga ciwon da ke da diamita mai tsayi. Ga waɗanda ake zargi da ƙarancin haɗarin GIST fiye da 2cm, idan an cire ƙwayar lymph ko metastasis mai nisa daga kimantawa kafin tiyatar, bisa ga tabbatar da cewa za a iya cire ciwon gaba ɗaya, ana iya yin tiyatar endoscopic ta hanyar ƙwararrun masu binciken endoscopic a cikin wani yanki mai fasahar maganin endoscopic mai girma.
ii. Mai nuna alamun cutar (misali, zubar jini, toshewar jini) SMT.
iii. Marasa lafiya waɗanda ake zargin cewa ciwon daji ba shi da lahani ta hanyar gwajin kafin tiyata ko kuma an tabbatar da shi ta hanyar cututtuka, amma ba za a iya bin diddiginsa akai-akai ba ko kuma waɗanda ciwon dajinsu ya ƙaru cikin ɗan gajeren lokaci a lokacin bin diddigin cutar kuma waɗanda ke da sha'awar gaske.e don maganin endoscopic.
(3) Hana Amfani da Magunguna
i. Gano raunukan da suka same nian yi masa ɗanɗano zuwa ƙwayoyin lymph ko wurare masu nisa.
ii. Ga wasu SMT tare da lymph mai tsabtanodeko kuma nesa da metastasis, ana buƙatar biopsy mai yawa don samun ilimin cututtuka, wanda za'a iya ɗaukarsa a matsayin contraindication na dangi.
iii. Bayan cikakken bayani kafin tiyatakimantawa, an tabbatar da cewa yanayin gabaɗaya ba shi da kyau kuma tiyatar endoscopic ba zai yiwu ba.
Raunuka marasa kyau kamar lipoma da pancreas na mahaifa ba sa haifar da alamu kamar ciwo, zubar jini, da toshewar hanyoyin jini.MT yana bayyana a matsayin zaizayar ƙasa, ciwon mara, ko kuma ƙaruwa cikin sauri cikin ɗan gajeren lokaci, yuwuwar zama mummunan rauni yana ƙaruwa.
(4)Zaɓin hanyar yankewad
Sake yanke tarko na endoscopic: DonSMT wanda yake a saman jiki, yana fitowa cikin rami kamar yadda gwaje-gwajen EUS da CT suka tabbatar kafin tiyata, kuma ana iya cire shi gaba ɗaya a lokaci guda ta hanyar amfani da tarko, ana iya amfani da hanyar cire tarko ta endoscopic.
Binciken cikin gida da na ƙasashen waje ya tabbatar da cewa yana da aminci kuma yana da tasiri a cikin SMT na sama sama da ƙasa da 2cm, tare da haɗarin zubar jini na 4% zuwa 13% da kuma hudawahaɗarin kashi 2% zuwa 70%.
Endoscopic submucosal haƙa rami, ESE: Ga SMTs masu tsayin diamita ≥2 cm ko kuma idan gwaje-gwajen hoto kafin tiyata kamar EUS da CT sun tabbatar da hakanIdan ciwon ya fito cikin ramin, ESE zai yiwu don cire sassan SMT masu mahimmanci na endoscopic.
ESE tana bin ƙa'idodin fasaha naAna yin tiyatar cirewar submucosal dissection (ESD) da kuma cirewar mucosal endoscopic, kuma ana amfani da yankewa mai zagaye "juyawa sama" a kusa da ciwon don cire mucosal da ke rufe SMT da kuma fallasa ciwon gaba ɗaya. , don cimma manufar kiyaye mutuncin ciwon, inganta tsauraran matakan tiyata, da kuma rage matsalolin da ake fuskanta a lokacin tiyata. Ga ciwon da ya kai ≤1.5 cm, ana iya cimma cikakken matakin cirewa na 100%.
Sake Gyaran Tushen Ruwa na Submucosalion, STER: Ga SMT da ya samo asali daga muscularis propria a cikin esophagus, hilum, ƙaramin lanƙwasa na jikin ciki, ƙoƙon ciki da dubura, waɗanda suke da sauƙin kafa ramuka, kuma diamita mai ratsawa shine ≤ 3.5 cm, STER na iya zama hanyar magani da aka fi so.
STER sabuwar fasaha ce da aka haɓaka bisa ga peroral endoscopic esophageal sphincterotomy (POEM) kuma faɗaɗa ce ta fasahar ESDNology. Yawan cirewar STER na en bloc don maganin SMT ya kai kashi 84.9% zuwa 97.59%.
Tsarin Endoscopic Cikakken kauriion,EFTR: Ana iya amfani da shi don SMT inda yake da wahala a kafa rami ko kuma inda matsakaicin diamita na ƙari ya kai ≥3.5 cm kuma bai dace da STER ba. Idan ciwon ya fito a ƙarƙashin membrane mai launin shunayya ko kuma ya girma a wajen wani ɓangare na ramin, kuma an gano cewa ciwon yana manne sosai da layin serosa yayin tiyata kuma ba za a iya raba shi ba, ana iya amfani da shi. EFTR yana yin maganin endoscopic.
Daidaitaccen dinki na ramin da aka hudaWurin da aka yi bayan EFTR shine mabuɗin nasarar EFTR. Domin a tantance haɗarin sake dawowar ƙari daidai da kuma rage haɗarin yaɗuwar ƙari, ba a ba da shawarar a yanke da cire samfurin ƙari da aka cire a lokacin EFTR ba. Idan ya zama dole a cire ƙari gunduwa-gunduwa, dole ne a fara gyara ramin don rage haɗarin shuka da yaɗuwar ƙari. Wasu hanyoyin ɗinki sun haɗa da: ɗinkin ƙarfe, ɗinkin tsotsa, dabarun ɗinkin fata, hanyar "dinkin jaka" ta igiyar nailan tare da ƙulle ƙarfe, tsarin rufe ƙarfe (ƙullewar ƙulle-ƙulle, OTSC) ɗinkin OverStitch da sauran sabbin fasahohi don gyara raunukan ciki da magance zubar jini, da sauransu.
(5) Matsalolin da suka biyo bayan tiyata
Zubar jini a lokacin tiyata: Zubar jini wanda ke sa sinadarin haemoglobin na majiyyaci ya ragu da fiye da 20 g/L.
Don hana zubar jini mai yawa a lokacin tiyata,Ya kamata a yi allurar submucosal isasshe a lokacin aikin don fallasa manyan jijiyoyin jini da kuma sauƙaƙe coagulation na lantarki don dakatar da zubar jini. Ana iya magance zubar jini a lokacin tiyata ta amfani da wukake daban-daban na yankewa, forceps na hemostatic ko ƙulle-ƙulle na ƙarfe, da kuma rigakafin zubar jini na jijiyoyin jini da aka fallasa da aka samu yayin aikin yankewa.
Zubar jini bayan tiyata: Zubar jini bayan tiyata yana bayyana ne ta hanyar amai da jini, melena, ko jini a cikin bayan gida. A cikin mawuyacin hali, girgizar jini na iya faruwa. Yawancin lokaci yana faruwa cikin mako 1 bayan tiyata, amma kuma yana iya faruwa makonni 2 zuwa 4 bayan tiyata.
Zubar jini bayan tiyata sau da yawa yana da alaƙa daAbubuwa kamar rashin ingantaccen tsarin rage hawan jini bayan tiyata da kuma tsatsawar sauran jijiyoyin jini ta hanyar sinadarin gastric acid. Bugu da ƙari, zubar jini bayan tiyata yana da alaƙa da wurin da cutar ta faru, kuma ya fi yawa a cikin ƙoƙon ciki da ƙananan dubura.
Jinkirin hudawa: Yawanci yana bayyana a matsayin kumburin ciki, ciwon ciki mai tsanani, alamun ciwon peritonitis, zazzabi, kuma gwajin hoto yana nuna tarin iskar gas ko ƙaruwar tarin iskar gas idan aka kwatanta da na baya.
Yawanci yana da alaƙa da abubuwa kamar rashin ɗinki na raunuka, yawan amfani da na'urar lantarki, tashi da wuri don motsawa, cin abinci da wuri, rashin sarrafa sukari a jini, da kuma lalacewar raunuka ta hanyar acid na ciki. a. Idan raunin ya yi girma ko zurfi ko kuma raunin yana da fis.Sauye-sauye masu kama da juna, ya kamata a tsawaita lokacin hutawa da lokacin azumi yadda ya kamata kuma a yi aikin rage matsewar ciki bayan tiyata (marasa lafiya bayan tiyatar ƙananan hanyoyin ciki ya kamata a yi magudanar ruwa ta dubura); b. Marasa lafiya masu ciwon sukari ya kamata su kula da sukarin jininsu sosai; waɗanda ke da ƙananan ramuka da ƙananan cututtukan ƙirji da ciki ya kamata a ba su magunguna kamar azumi, hana kamuwa da cuta, da kuma rage acid; c. Ga waɗanda ke da kumburin ƙirji, za a iya yin magudanar ƙirji da huda ciki. Ya kamata a sanya bututu don kula da magudanar ruwa mai santsi; d. Idan ba za a iya gano kamuwa da cutar ba bayan magani mai kyau ko kuma an haɗa shi da kamuwa da cutar ƙirji mai tsanani, ya kamata a yi aikin laparoscopy na tiyata da wuri-wuri, kuma a yi gyaran magudanar ruwa da magudanar ruwa na ciki.
Matsalolin da suka shafi iskar gas: Har da subcutaciwon huhu (neous emphysema), ciwon huhu (pneumomediastinum), ciwon huhu (pneumothorax) da kuma ciwon huhu (pneumoperitoneum).
Ciwon emphysema na subcutaneous a lokacin tiyata (wanda aka nuna a matsayin emphysema a fuska, wuya, bangon ƙirji, da kuma scrotum) da kuma ciwon huhu na mediastinal (s).Ana iya samun kumburin epiglottis yayin aikin gastroscopy) yawanci ba ya buƙatar magani na musamman, kuma emphysema gabaɗaya zai warware da kansa.
Babban pneumothorax yana faruwa dtiyatar uring [matsin iska ya wuce 20 mmHg yayin tiyata
(1mmHg=0.133kPa), SpO2 <90%, wanda aka tabbatar ta hanyar X-ray na gaggawa a gefen gado], ana iya ci gaba da tiyatar bayan an rufe tiyatar ƙirjiinage.
Ga marasa lafiya da ke da cutar pneumoperitoneum a lokacin tiyata, yi amfani da allurar pneumoperitoneum don huda wurin McFarlanda cikin ƙananan ciki na dama don fitar da iskar, sannan a bar allurar huda a wurin har zuwa ƙarshen aikin, sannan a cire ta bayan an tabbatar da cewa babu wani iskar gas da ke fitowa.
Fistula na hanji: Ruwan narkewar abinci wanda tiyatar endoscopic ke haifarwa yana shiga cikin ƙirji ko ramin ciki ta hanyar zubewa.
Fistulas na tsakiyar esophageal da fistulas na esophagothoracic sun zama ruwan dare. Da zarar fistula ta faru, a rufe magudanar ƙirji don a kula da ita.a cikin magudanar ruwa mai santsi kuma a samar da isasshen tallafin abinci mai gina jiki. Idan ya cancanta, ana iya amfani da maƙullan ƙarfe da na'urorin rufewa daban-daban, ko kuma a sake amfani da cikakken murfin. Ana amfani da maƙullan ƙarfe da sauran hanyoyi don toshe magudanar ruwaCiwon fistula. Mummunan yanayi yana buƙatar gaggawar tiyata.
3. Kulawa bayan tiyata (fmai laushi)
(1) Raunuka masu kyau:Cututtuka syana nuna cewa raunuka marasa lahani kamar lipoma da leiomyoma ba sa buƙatar kulawa akai-akai.
(2) SMT ba tare da cutarwa bayuwuwar tururuwa:Misali, ya kamata a yi cikakken tsarin gwajin jini na dubura mai tsawon 2cm, da kuma gwajin jini na matsakaici da babban haɗari (GIST), sannan a yi la'akari da ƙarin jiyya (tiyata, maganin chemotherapy, maganin da aka yi niyya). Tsarin tsarin ya kamata ya dogara ne akan shawarwari da dama da kuma mutum ɗaya.
(3) Ƙananan yiwuwar cutar SMT:Misali, ana buƙatar a tantance GIST mai ƙarancin haɗari ta hanyar EUS ko ɗaukar hoto duk bayan watanni 6 zuwa 12 bayan magani, sannan a yi masa magani bisa ga umarnin asibiti.
(4) SMT mai matsakaicin ƙarfi da kuma babban yuwuwar cutarwa:Idan cututtukan bayan tiyata sun tabbatar da nau'in NET na ciki na 3, NET na hanji mai tsayi sama da 2cm, da kuma GIST mai matsakaicin da babban haɗari, ya kamata a yi cikakken tsari kuma a yi la'akari da ƙarin jiyya (tiyata, maganin chemotherapy, maganin da aka yi niyya). Tsarin shirin ya kamata ya dogara ne akan[game da mu 0118.docx] shawarwari da dama da kuma bisa ga mutum ɗaya.
Mu, Jiangxi Zhuoruihua Medical Instrument Co., Ltd., kamfani ne da ke kera kayayyaki a China wanda ya ƙware a fannin amfani da endoscopic, kamar suƙarfin biops, hemoclip, tarkon polyp, allurar sclerotherapy, feshi catheter, gogewar cytology, waya mai jagora, Kwandon ɗaukar dutse, catheter na magudanar ruwa ta hancida sauransu waɗanda ake amfani da su sosai a cikinEMR, ESD,ERCPKayayyakinmu an ba su takardar shaidar CE, kuma masana'antunmu an ba su takardar shaidar ISO. An fitar da kayayyakinmu zuwa Turai, Arewacin Amurka, Gabas ta Tsakiya da wani ɓangare na Asiya, kuma yana sa abokin ciniki ya yaba da kuma yaba masa sosai!
Lokacin Saƙo: Janairu-18-2024